
Evidence Mounts for Greater COVID Prevalence

Researchers hoping to figure out that number have been using antibody tests and other data to try and figure out who’s been exposed. As more data come to light, researchers hope it will help shape policies around social distancing guidelines as officials look to reopen the country.
Gathering the Numbers
Hard-hit New York, the first state to do its own antibody testing, found an estimated 13.9% prevalence rate statewide, Gov. Andrew Cuomo said Thursday. The rate was even higher in New York City, at 21.2%.
The state randomly tested 3,000 people who were out shopping. Cuomo said the results may be high because they tested people who were out, not people who are isolating at home.
These early figures would lower the fatality to infection rate to .5%, Cuomo said. But he cautioned that the data is preliminary and that current fatality rates will go higher because they don’t include at-home deaths.
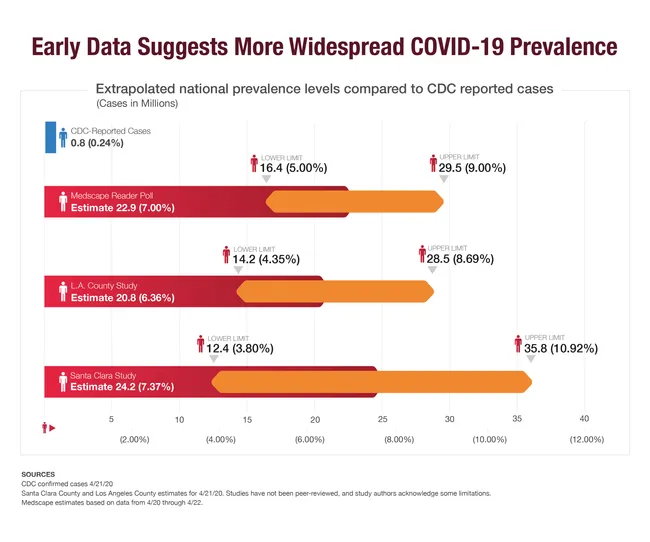
Earlier this week, one of the first studies based on antibody tests caused an uproar this week, when preliminary results suggested that more than 50 times as many people had been infected as had tested positive in Santa Clara County, CA. The study hasn’t yet been peer reviewed, and statisticians pointed out numerous flaws in the interpretation of the data.
Preliminary results from the first round of another antibody study, though, reached a similar number. This one, from USC and the Los Angeles County Department of Public Health, found that the real number of infected people in LA County would be 28 to 55 times higher than diagnostic testing showed.
“The estimates also suggest that we might have to recalibrate disease prediction models and rethink public health strategies,” said lead investigator Neeraj Sood, professor of public policy at the USC Price School for Public Policy and senior fellow at the USC Schaeffer Center for Health Policy and Economics in a news release.
While these studies are the first to use antibodies, anecdotal information also suggests the virus has reached far more people than we know. Rochelle Walensky, MD, chief of the Division of Infectious Diseases at Massachusetts General Hospital and Brigham and Women’s Hospital, shared some surprising local results. To make room for more COVID patients, Brigham and Women’s wanted to empty their subacute nursing facility. Before releasing those patients, though, they had to be tested. Out of 87 patients total, 50 tested positive—and none had shown any symptoms.
Also in Boston, at one homeless shelter none of the 146 people who tested positive had any symptoms. Aboard the aircraft carrier USS Theodore Roosevelt, 600 crewmembers have tested positive, but at least 350 of them are asymptomatic. In an Ohio prison that did widespread testing, 73% of inmates—more than 1,800 people—were
confirmed to have the virus, many without symptoms.
A report that relied upon CDC data for people with influenza-like illnesses estimates that at least 8.7 million people were infected with coronavirus during a three-week period in March. And a new analysis of widespread testing in the town of Vo, Italy, found that 43% of people who tested positive showed no symptoms. Neither report has yet been peer reviewed.
A Medscape reader poll of 1,451 U.S. physicians found that 80% believe the proportion of people infected with COVID-19 is “generally higher than what has been reported.” Still, just under half responded that fewer than 5% of people around the world have been infected, with approximately one in five U.S. physicians responding that they believe the figure is between 3% and 4%.
A WebMD reader poll of more than 6,300 visitors found that 10% of the respondents suspected they had COVID-19 during the past 30 days, yet only 7% were diagnosed officially through a test.
Applying the Numbers
Amesh Adalja, MD, of the Johns Hopkins University Center for Health Security, agrees that if the prevalence of coronavirus is really this much larger than the confirmed cases show, that means it’s much less deadly than we thought -- and if you do get it, your chances of being hospitalized are lower.
He says we should expect the coronavirus to be widespread. “The point people are forgetting is, it’s a community-spreading respiratory virus,” says Adalja. “If you look back at H1N1 in 2009, that was a novel flu virus. Within one year it infected 1 billion people.”
Even if we had a confirmation of how many people have been infected, that wouldn’t necessarily mean we can start going back to our normal lives. A larger number of people who show no symptoms means more could potentially spread the disease.
“If we relax any restrictions, we're going to get more cases, because this virus isn’t going anywhere until there’s a vaccine,” says Adalja.
Cuomo said his state’s antibody tests would be ongoing, and tracking the infection rate would help him make decisions about distancing guidelines. If the state relaxes restrictions and the rate starts rising again, for instance, he might have to revise the guidelines.
One of the problems with a new virus is that nobody has any natural immunity. To achieve herd immunity, upwards of 60% of the population would need to have been infected. The Santa Clara study found only 2.5% to 4.2% of residents had been. The USC/LA County study showed about 2.8% to 5.6% of the county’s adult population has an antibody to the virus. The World Health Organization, too, reached a similar conclusion from preliminary data: 2% to 3% of the world’s population has developed antibodies.
Relying on antibody studies poses another problem. “We don’t even know if having antibodies is protective, short term or long term,” says Denis Nash, PhD, MPH, Executive Director of the CUNY Institute for Implementation Science in Population Health in New York. So even if tests show you have antibodies, it may be possible to get re-infected. “We may not be able to achieve herd immunity without a vaccine.”
Before deciding to ease any restrictions, we should be looking at different statistics, including the death rate, Nash says.
That number of fatalities has also been underestimated. Until recently, states only reported a death from COVID-19 only when someone had tested positive. But the CDC last week updated its guidance to now include both confirmed cases and probable ones. When New York added probable cases, the numbers rose by 3,700 from the beginning of the outbreak.
“Until you start to see a decline in the death rate, and the number in ICU comes down to a manageable level, you can’t think about relaxing social and physical distancing restrictions,” said Nash. “And when or if you do relax, you need to be ready to detect when things tick back up, so you can turn those strategies back on. You need the ability to do more testing and contact tracing.”
For most areas of the country, those goals haven’t been met. Yet.
SOURCE:
Sources
Article: Evidence Mounts for Greater COVID Prevalence
CNN: “Iceland lab's testing suggests 50% of coronavirus cases have no symptoms,” “'We need to fix it quickly.' Asymptomatic coronavirus cases at Boston homeless shelter raise red flag.”
Johns Hopkins University: “COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU).”
MedRxiv: “COVID-19 Antibody Seroprevalence in Santa Clara County, California,” “Suppression of COVID-19 outbreak in the municipality of Vo, Italy.”
Mercury News: “Feud over Stanford coronavirus study: ‘The authors owe us all an apology.’”
USC: “Early antibody testing suggests COVID-19 infections in L.A. County greatly exceed documented cases.”
Rochelle Walensky, MD, chief, Division of Infectious Diseases, Massachusetts General Hospital and Brigham and Women’s Hospital; professor, Harvard Medical School.
Navy Times: “SECDEF: Majority of Roosevelt sailors with COVID-19 are asymptomatic.”
NPR: “73% Of Inmates At An Ohio Prison Test Positive For Coronavirus.”
Amesh Adalja, MD, senior scholar, Johns Hopkins University Center for Health Security.
Denis Nash, PhD, executive director, CUNY Institute for Implementation Science in Population Health; distinguished professor of epidemiology, CUNY School of Public Health.
News briefing, World Health Organization, April 20, 2020.
News briefing, Infectious Diseases Society of America, April 17, 2020.
CDC: “Guidance for Certifying Deaths Due to Coronavirus Disease 2019 (COVID-19).”
WebMD poll of 6,343 readers to the homepage on desktop and mobile, April 20-21, 2020.
News briefing, New York Gov. Andrew Cuomo, April 23, 2020.
Medscape doctor poll, conducted online, April 20 through April 22, 2020. Results based on 5,300 Medscape member doctors (1,451 U.S. doctors, 3,849 non-U.S. doctors).
You Might Also Enjoy...


How NightLase® Can Help With Snoring

How Laser Therapy Can Help Decrease Vaginal Dryness and Increase Sexual Pleasure

Five Signs You Could Be Suffering From Low Testosterone

Why Do I Still Get Acne, and How Can I Get Rid of It Without Medication?

